
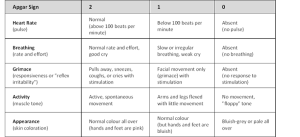

Variables associated with immediate ICU admissionĪccording to the multivariate logistic regression model, age, sex, ASA classification, emergency surgery, and SAS were associated with the ICU admission rate (Table 3). As the SAS decreased from 9–10 to 0–1, the frequency of ICU admission progressively increased from 3.2 to 46.2% (P < 0.001, Table 2). The type of operation also affected the rates of ICU admission, and more than half of the patients who underwent cardiovascular surgery and almost half of those who underwent thoracic surgery were admitted to the ICU immediately, whereas none of the patients who underwent obstetric, ophthalmic, dental, or pain-related procedures were admitted to the ICU (Table 1). Factors associated with a higher frequency of ICU admission included older age, male sex, emergency surgery, and higher ASA class. There were statistically significant differences in the patient characteristics between the groups of patients who were and were not immediately admitted to the ICU (Table 2). In this cohort, 1020 patients (7.8%) were transferred directly from the operating room or post-anesthesia care unit (PACU) to the ICU after the operation. The SAS was positively correlated with postoperative complications and/or mortality 7 in patients undergoing vascular surgery, 8 noncardiac surgery 9, general surgery 8, esophagectomy 10, colorectal resection 11, emergency abdominal surgery 12, elective laparoscopic cholecystectomy 13, hepatectomy for hepatocellular carcinoma 14, liver transplantation 15, general oncologic surgery 8, 16, 17, laparotomy gynecological surgery 18, radical or partial nephrectomy for renal mass excision 19, radical protectomy 20, hip or knee arthroplasty 21, transfemoral amputation 22, lumbar fusion for degenerative spine diseases 23, intracranial meningioma 24, and head and neck cancer 13, 25.įull size table Frequency of admission to ICU The surgical Apgar score (SAS), which has been widely discussed over the past 10 years, is a simple formula that uses intraoperative hemodynamics and blood loss to predict the postoperative complications and mortality rate (Table 1) 6. Previous studies have reported indicators based on retrospective analyses of pediatric patients or specific surgeries, such as major pulmonary resection, urologic surgery, joint replacement, emergency operation, and degenerative spinal surgery 6, 7, 8, 9, 10, 11, but none of these indicators can be generally applied.

Thus, adopting adequate criteria for ICU admission is crucial. Unplanned postoperative ICU admission (i.e., ICU admission is not part of the preoperative plan) was associated with a significantly higher rate of mortality 3, 4 however, ICU admission without any clear indications may increase the postoperative hospital length of stay and associated costs 5. Patients who received intensive care immediately following the operation had a lower level of morbidity 3. Previous studies have shown that patients undergoing high-risk surgeries account for more than 80% of postoperative deaths nevertheless, less than 15% were admitted to the intensive care unit (ICU) immediately after the operation 2. In Taiwan, more than 14.9 million patients underwent surgery in 2015, including 4.6 million who underwent in-hospital surgeries 1. Although the SAS is calculated intraoperatively, it is a powerful tool for clinical decision-making regarding the immediate postoperative ICU transfer. In general, a higher ASA classification and a lower SAS were associated with higher rates of postoperative ICU admission after all surgeries. The odds ratios for ICU admission in patients with SASs of 0–2, 3–4, and 5–6 were 5.2, 2.26, and 1.73, respectively (P < 0.001). Age, sex, American Society of Anesthesiologists (ASA) class, emergency surgery, and the SAS were associated with ICU admission. Patients transferred to the ICU immediately after surgery was 7.8%. All patients undergoing operative anesthesia were retrospectively enrolled. Our study was performed to determine the relationship between the SAS and postoperative ICU transfer after all surgeries. The surgical Apgar score (SAS) (0–10) can be used to predict postoperative complications, mortality rates, and ICU admission after high-risk intra-abdominal surgery. Nevertheless, less than 15% of such patients are immediately admitted to the ICU due to no reliable criteria for admission. Immediate postoperative intensive care unit (ICU) admission can increase the survival rate in patients undergoing high-risk surgeries.


 0 kommentar(er)
0 kommentar(er)
